Åreforkalkning, aterosklerose
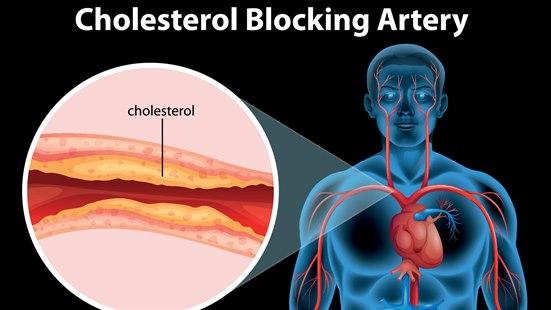
Aterosklerose er avleiringer av kolesterol på innsiden av arteriene. Aterosklerosen øker med mengden kolesterol og mettet fett i kosten. Risikoen for å ha aterosklerose gjenspeiles i blodets kolesterolinnhold og øker med alderen.
Sist oppdatert:
2. juli 2020
Aterosklerose
Arterier
Arteriene er de blodårene som frakter blod fra hjertet til resten av kroppen. Når du er ung og frisk, har arteriene en glatt innside, og de er elastiske nok til å tilpasse seg store blodtrykksvariasjoner, slik at blodet passerer fritt gjennom blodåren.
Aterom og plakk
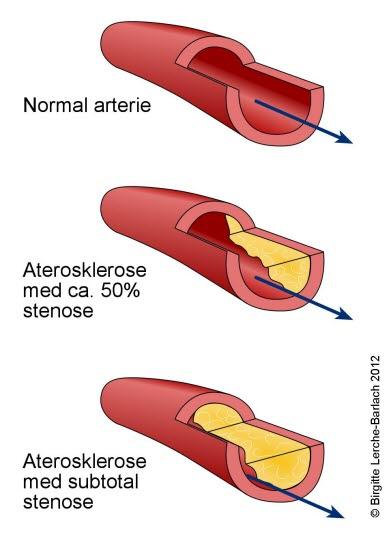
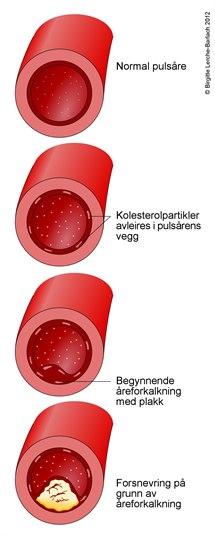
Noen ganger oppstår fettavleiringer på innsiden av arteriene. Disse avleiringene starter ofte på steder der arterien deler seg, eller der innsiden av karveggen (endotelet) er noe skadet. En slik fettavleiring betegnes et aterom. Et plakk er en stor aterom-masse. Utviklingen av et plakk starter med at kolesterol "graver" seg inn i veggen på blodåren. Kroppen forsøker å reparere denne skaden, det dannes arrvev som gjør karveggen tykkere og stivere og innvendig blir blodåren smalere. Ettersom mer kolesterol avleires, blir blodstrømmen inne i karet stadig dårligere. Dette betegnes i medisinsk terminologi for aterosklerose og er blant annet årsaken til koronar hjertesykdom.
Dette dokumentet er basert på det profesjonelle dokumentet Hjerteinfarkt . Referanselisten for dette dokumentet vises nedenfor
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018; 39: 119-77. doi:10.1093/eurheartj/ehx393 DOI
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J 2019; 40: 237-69. doi:10.1093/eurheartj/ehy462 DOI
- Reynolds HR, Maehara A, Kwong RY, et al. Coronary optical coherence tomography and cardiac magnetic resonance imaging to determine underlying causes of MINOCA in women. Circulation 2020. PMID: 33191769 PubMed
- Folkehelseinstituttet. Forekomst av hjerte- og karsykdom i 2018. Hjerte- og karregisteret. www.fhi.no
- Mehta S, Yusuf S. Acute myocardial infarction. In: Clinical evidence, issue 6. BMJ Publishing Group, 2000.
- Smolina K, Wright FL, Rayner M, Goldacre MJ. Determinants of the decline in mortality from acute myocardial infarction in England between 2002 and 2010: linked national database study. BMJ 2012; 344: d8059. BMJ (DOI)
- Albrektsen G, Heuch I, Løchen M-L, et al. Lifelong gender gap in risk of incident myocardial infarction. The Tromsø Study. JAMA Intern Med 2016; 176: 1673-9. pmid:27617629 PubMed
- Folkehelseinstituttet. Dødsfall etter hjerteinfarkt og hjerneslag er dramatisk redusert. Dødsårsaksregisteret. Publisert 04.12.2019 www.fhi.no
- Norsk hjerteinfarktregister. Årsrapport 2016. stolav.no
- Jortveit J, Govatsmark RES, Digre TA, et al. Hjerteinfarkt i Norge 2013. Tidsskr Nor Legeforen 2014; 134: 1841-6. Tidsskrift for Den norske legeforening
- Statistisk sentralbyrå. Dødsårsaksregister.
- Kodama S, Saito K, Tanaka S, Maki M, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women. A meta-analysis. JAMA 2009; 301: 2024 - 35. Journal of the American Medical Association
- Anderssen SA, Hjermann I. Fysisk aktivitet - en sentral faktor i forebyggingen av hjerte- og karsykdom. Tidsskr Nor Lægeforen 2000; 120: 3168-72. PubMed
- Murabito JM, Pencina MJ, Nam BH, et al. Sibling cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults. JAMA. 2005; 294: 3117-23. PubMed
- Gotto AM jr., LaRosa JC, Hunninghake D, Grundy SM, Wilson PW, Clarkson TB et al. The cholesterol facts. A summary of the evidence relating dietary fats, serum cholesterol, and coronary heart disease. A joint statement by the American Heart Association and the National Heart, Lung and Blood Institute. Circulation 1990; 81: 1721-33. Circulation
- Kamstrup PR, Tybjærg-Hansen A, Steffensen R, Nordestgaard BG. Genetically elevated lipoproten(a) and increased risk of myocardial infarction. JAMA 2009; 301: 2331-9. Journal of the American Medical Association
- Kessous R, Shoham-Vardi I, Pariente G, et al. Long-term maternal atherosclerotic morbidity in women with pre-eclampsia. Heart 2014. doi:10.1136/heartjnl-2014-306571 DOI
- Fowler G. Tobacco and cardiovascular disease: achieving smoking cessation . I: Yusuf S, red. Evidence based cardiology. London: BMJ Books, 1998: 179-90.
- Yusuf S, Hawken S, Ounpuu S, et al; INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364: 937-52. PubMed
- Lakka H-M, Lakka TA, Tuomilehto J, Salonen JT. Abdominal obesity is associated with increased risk of acute coronar events in men. Eur Heart J 2002; 23: 706-13. PubMed
- Bogers RP, Bemelmans WJ, Hoogenveen RT, et al. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: A meta-analysis of 21 cohort studies including more than 300 000 persons. Arch Intern Med 2007; 167: 1720-8. PubMed
- Hsia J, Larson JC, Ockene JK, et al. Resting heart rate as a low tech predictor of coroanary events in women: prospective cohort study. BMJ 2009; 338: b219. BMJ (DOI)
- Schjerning Olsen A, Fosbøl L, Lindhardsen J, et al. Long-term cardiovascular risk of NSAID use according to time passed after first-time myocardial infarction. A nationwide cohort study. Circulation 2012. doi:10.1161/CIRCULATIONAHA.112.112607
- Lindhardsen J, Ahlehoff O, Gislason GH, et al. The risk of myocardial infarction in rheumatoid arthritis and diabetes mellitus: a Danish nationwide cohort study. Ann Rheum Dis 2011; 70: 929-934. PubMed
- Mehta NN, Yu Y, Pinnelas R, et al. Attributable risk estimate of severe psoriasis on major cardiovascular events. Am J Med 2011; 124: 775. PubMed
- Ruidavets J-B, Ducimetiére P, Evans A, et al. Patterns of alcohol consumption and ischaemic heart disease in culturally divergent countries: the Prospective Epidemiological Study of Myocardaial Infarction (PRIME). BMJ 2010; 341: c6077. BMJ (DOI)
- Kwong JC, Schwartz KL, Campitelli MA, et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med 2018; 378: 345-53. pmid:29365305 PubMed
- McSweeney JC, Cody M, Sullivan P, et al. Women's early warning symptoms of acute myocardial infarction. Circulation 2003; 108: 2619-23. Circulation
- Lichtman JH, Leifheit EC, Safdar B, et al. Sex differences in the presentation and perception of symptoms among young patients with myocardial infarction: Evidence from the VIRGO study (Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients. Circulation 2018; 137: 781. pmid:29459463 PubMed
- Ammann P, Pfisterer M, Fehr T, Rickli H. Raised cardiac troponins. BMJ 2004; 328: 1028-9. PubMed
- Bischof JE, Worrall C, Thompson P, et al. ST depression in lead aVL differentiates inferior ST-elevation myocardial infarction from pericarditis. Am J Emerg Med 2016. PMID: 26542793 PubMed
- Maffei E, Seitun S, Martini C, et al. CT coronary angiography and exercise ECG in a population with chest pain and low-to-intermediate pre-test likelihood of coronary artery disease. Heart 2010; 96: 1973-9 PubMed
- Valgimigli M, Frigoli E, Leonardi S, et al. Bivalirudin or unfractionated heparin in acute coronary syndromes. N Engl J Med 2015; 373:997. DOI: 10.1056/NEJMoa1507854 DOI
- Bøhmer E, Hoffmann P, Abdelnoor M, et al. Efficacy and safety of immediate angioplasty versus ischemia-guided management after thrombolysis in acute myocardial infarction in areas with very long transfers. J Am Coll Cardiol 2009; : PMID:19747792. PubMed
- Siemieniuk RAC, Chu DK, Kim LH, et al. Oxygen therapy for acutely ill medical patients: a clinical practice guideline. BMJ 2018; 363: k4169. pmid:30355567 PubMed
- Sepehrvand N, James SK, Stub D, et al. Effects of supplemental oxygen therapy in patients with suspected acute myocardial infarction: a meta-analysis of randomised clinical trials. Heart 2018. pmid:29599378 PubMed
- Cabello JB, Burls A, Emparanza JI, Bayliss SE, Quinn T. Oxygen therapy for acute myocardial infarction. Cochrane Database of Systematic Reviews 2016, Issue 12. Art. No.: CD007160. DOI: 10.1002/14651858.CD007160.pub4. DOI
- Grønvold T, Evang JA, Stensæth KH. En 51 år gammel kvinne med akutte brystsmerter. Tidsskr Nor Legeforen 2008; 128: 2836-8. Tidsskrift for Den norske legeforening
- Morrison LJ, et al. Mortality and prehospital thrombolysis for acute myocardial infarction. JAMA 2000; 283: 2686-92. Journal of the American Medical Association
- Hole T, Juvkam PC, Lied A. Primærlegebasert prehospital trombolytisk behandling ved akutt hjarteinfarkt. Tidsskr Nor Lægeforen 2005; 125: 1486-8. PubMed
- Roffi M, Patrono C, Collet J-P, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016; 37: 267-315. doi:10.1093/eurheartj/ehv320 DOI
- Choo EH, Chang K, Ahn Y, et al. Benefit of β-blocker treatment for patients with acute myocardial infarction and preserved systolic function after percutaneous coronary intervention. Heart 2013. doi:10.1136/heartjnl-2013-305137 DOI
- Bangalore S, Makani H, Radford M, et al. Clinical Outcomes with beta-Blockers for Myocardial Infarction: A Meta-analysis of Randomized Trials. Am J Med. 2014 Oct;127(10):939-53. PubMed
- Reikvam Å, Madsen S. Hvordan skal ACE-hemmere brukes ved hjerteinfarkt? Tidsskr Nor Lægeforen 2000; 120: 3413-7. Tidsskrift for Den norske legeforening
- Pitt B, White H, Nicolau J, et al. Eplerenone reduces mortality 30 days after randomization following acute myocardial infarction in patients with left ventricular systolic dysfunction and heart failure. J Am Coll Cardiol 2005; 46: 425-31. PubMed
- Ezekowitz JA, McAlister FA. Aldosteron blockade and left ventricular dysfunction: a systematic review of randomized clinical trials. Eur Heart J 2009; 30: 469-77. European Heart Journal
- Bøtker HE, Kharbanda R, Schmidt MR, et al. Remote ischemic conditioning before hospital admission, as a complement to angioplasty, and effect on myocardial salvage in patients with acute myocardial infarction: a randomised trial. Lancet 2010; 375: 727-34. PubMed
- Pryds K, Terkelsen CJ, Sloth AD, et al. Remote ischaemic conditioning and healthcare system delay in patients with ST-segment elevation myocardial infarction. Heart 2016. doi:10.1136/heartjnl-2015-308980 DOI
- Hausenloy DJ, Kharbanda RK, Møller UK, et al. Effect of remote ischaemic conditioning on clinical outcomes in patients with acute myocardial infarction (CONDI-2/ERIC-PPCI): a single-blind randomised controlled trial. Lancet 2019. doi:10.1016/S0140-6736(19)32039-2 DOI
- Fernández-Bergés D, Degano IR, Fernandez RG, et al. Benefit of primary percutaneous coronary interventions in the elderly with ST segment elevation myocardial infarction. Open Heart 2020. doi:10.1136/openhrt-2019-001169 DOI
- Hochman JS, Lamas GA, Buller CE, et al. Coronary intervention for persistent occlusion after myocardial infarction. N Engl J Med 2006; 355: 2395-2407. New England Journal of Medicine
- Vik-Mo H. Warfarin saman med blodplatehemming. Tidsskr Nor Legeforen 2011; 131: 252-3. Tidsskrift for Den norske legeforening
- O'Donoghue ML, Murphy SA, Sabatine MS. The safety and efficacy of aspirin discontinuation on a background of a P2Y12 inhibitor in patients after percutaneous coronary intervention: A systematic review and meta-analysis. Circulation 2020 Jun 19; doi: 10.1161/CIRCULATIONAHA.120.046251 DOI
- Yin SH, Xu P, Wang B, et al. Duration of dual antiplatelet therapy after percutaneous coronary intervention with drug-eluting stent: systematic review and network meta-analysis. BMJ 2019; 365: l2222. pmid:31253632 PubMed
- Sørensen R, Hansen ML, Abildstrom SZ, et al. Risk of bleeding in patients with acute myocardial infarction treated with different combinations of aspirin, clopidogrel, and vitamin K antagonists in Denmark: a retrospective analysis of nationwide registry data. Lancet 2009; 374: 1967-74. PubMed
- Hohnloser SH, Kuck KH, Dorian P, et al. Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction. N Engl J Med 2004; 351: 2481-88. New England Journal of Medicine
- Jolly SS, Cairns JA, Yusuf S, et al. Randomized trial of primary PCI with or without routine manual thrombectomy. N Engl J Med 2015. doi:10.1056/NEJMoa1415098 DOI
- Jolly SS, Cairns JA, Yusuf S, et al. Outcomes after thrombus aspiration for ST elevation myocardial infarction: 1-year follow-up of the prospective randomised TOTAL trial. Lancet 2015. doi:10.1016/S0140-6736(15)00448-1 DOI
- Rizos EC, Ntzani E, Bika E, et al. Association between omega-3 fatty acid supplementation and risk of major cardiovascular disease events. JAMA 2012; 308: 1024-33. Journal of the American Medical Association
- Chowdhury R, Warnakula S, Kunutsor S, et al. Association of dietary, circulating, and supplement fatty acids with coronary risk: A systematic . Ann Intern Med 2014; 160: 398-406. doi:10.7326/M13-1788 DOI
- Sesso HD, Christen WG, Bubes V, et al. Multivitamins in the Prevention of Cardiovascular Disease in Men: The Physicians` Health Study II Randomized Controlled Trial. JAMA 2012 Nov 7; 308(17): 1751-60. PubMed
- Jenkins DJA, Spence JD, Giovannucci EL, et al. Supplemental Vitamins and Minerals for CVD Prevention and Treatment. J Am Coll Cardiol. 2018 Jun 5;71(22):2570-2584. PMID: 29852980. PubMed
- Gulliksson M, Burell G, Vessby B, et al. Randomized Controlled Trial of Cognitive behavioral therapy vs standard treatment to prevent recurrent cardiovascular events in patients with coronary heart disease. Arch Intern Med 2011; 171: 134-40. PubMed
- Levine GN, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease. Circulation 2016. doi:10.1161/CIR.0000000000000404 DOI
- Helsedirektoratet. Nasjonal faglig retningslinje for forebygging av hjerte- og karsykdom. Helsedirektoratet, 2017 www.helsedirektoratet.no
- Kim J, Kang D, Park H, et al. Long-termβ-blocker therapy and clinical outcomes after acute myocardial infarction in patients without heart failure: nationwide cohort study. Eur Heart J 2020; 41: 3521. pmid:32542362 PubMed
- Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med 2017. pmid:28304224 PubMed
- Guedeney P, Giustino G, Sorrentino S, et al. Efficacy and safety of alirocumab and evolocumab: a systematic review and meta-analysis of randomized controlled trials. Eur Heart J. 2019 Jul 3. pii: 5527995. PMID: 31270529 PubMed
- Udell JA, Zawi R, Bhatt DL, et al. Association between influenza vaccination and cardiovascular outcomes in high-risk patients: a meta-analysis. JAMA 2013 Oct 23;310(16):1711-20. PubMed
- Ridker PM, Everett BM, Thuren T, et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N Engl J Med 2017. doi:10.1056/NEJMoa1707914 DOI
- Tardif JC, Kouz S, Waters DD, et al. Efficacy and Safety of Low-Dose Colchicine after Myocardial Infarction. N Engl J Med 2019. PMID: 31733140 PubMed
- Cucherat M, Bonnefoy E, Tremeau G. Primary angioplasty versus intravenous thrombolysis for acute myocardial infarction. Oxford: The Cochrane Library, issue 2, 2002. The Cochrane Library
- Anderson L, Thompson DR, Oldridge N, Zwisler AD, Rees K, Martin N, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database of Systematic Reviews 2016, Issue 1. Art. No.: CD001800. DOI: 10.1002/14651858.CD001800.pub3 DOI
- Campell NC, Thain J, Deans HG et al. Secondary prevention clinics for coronary heart disease: randomised trial of effect on health. BMJ 1998; 316: 1434-7. British Medical Journal
- Murchie P, Campbell NC, Ritchie LD et al. Secondary prevention clinics for coronary heart disease: four year follow up of a randomised controlled trial in primary care. BMJ 2003; 326: 84-9. British Medical Journal
- Dalal HM, Zawada A, Jolly K, Moxham T, Taylor RS. Home based versus centre based cardiac rehabilitation: Cochrane systematic review and meta-analysis. BMJ 2010; 340: b5631. BMJ (DOI)
- Solomon SD, Zelenkofske S, McMurray JJ, et al, for the Valsartan in Acute Myocardial Infarction Trial (VALIANT) Investigators. Sudden death in patients with myocardial infarction and left ventricular dysfunction, heart failure, or both. N Engl J Med 2005; 352: 2581-8. New England Journal of Medicine
- Lichtman JH, Bigger JT, Blumenthal JA et al. Depression and coronary heart disease. Circulation 2008; 118: .
- Folkehelseinstituttet. Kvalitet i helsetjenesten. 30 dagers overlevelse og reinnleggelse etter sykehusinnleggelse. Resultater for 2019. FHI 2020. www.fhi.no
- Vaccarino V, Parsons L, Peterson ED, et al. Sex differences in mortality after acute myocardial infarction. Arch Intern Med 2009; 169: 1767-74. PubMed
- Vik-Mo H, Slette M, Hegbom K. Antitrombotisk behandling etter perkutan koronar intervensjon med stent. Tidsskr Nor Legeforen 2008; 128: 436-9. PubMed
- Budaj A, Yusuf S, Mehta SR, Fox KA, Tognoni G, Zhao F, et al. Benefit of clopidogrel in patients with acute coronary syndromes without ST-segment elevation in various risk groups. Circulation 2002;106:1622-6. Circulation